Countries whose health systems differ greatly reveal the complex interplay of culture, politics, and economics in shaping healthcare delivery. For instance, universal models in Canada and Sweden reduce disparities by ensuring wide access, while privatized systems like in the U.S. often create barriers for low-income individuals. Hybrid approaches blend public and private elements, enhancing care access and patient engagement. A closer look at metrics like life expectancy and patient satisfaction highlights how these systems perform. By examining these diverse approaches, you'll uncover valuable insights into effective healthcare strategies worldwide.
Overview of Global Health Systems
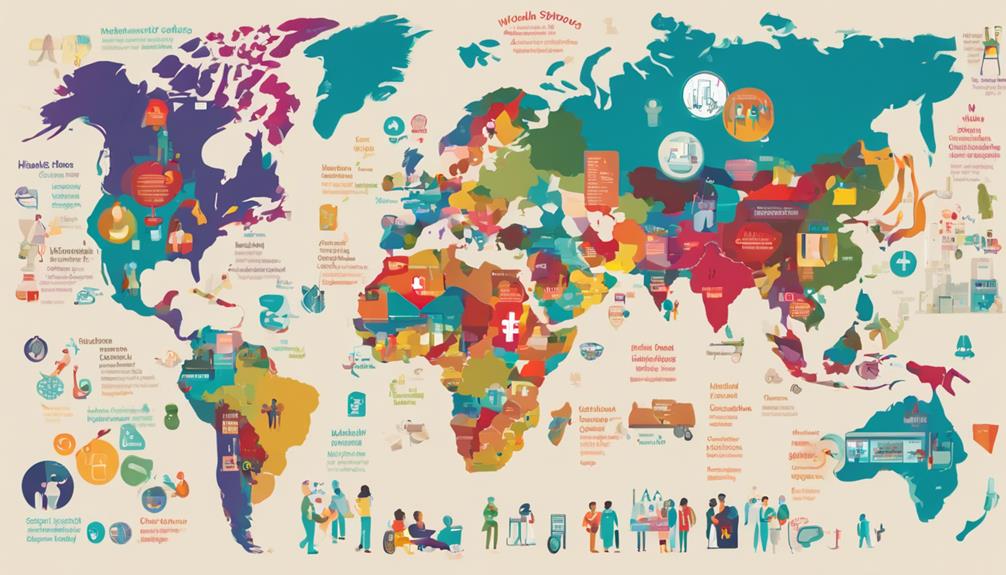
Global health systems operate under a variety of models, each shaped by unique political, economic, and cultural contexts that influence access, quality, and efficiency of care. These systems play a vital role in addressing global health disparities, which persist despite advancements in medicine and technology.Medicaid Mental HealthTenncare Dental For AdultsUnitedhealthcare Dental Medicaid
You'll notice that countries with robust healthcare financing mechanisms often demonstrate better health outcomes. In contrast, nations facing healthcare financing challenges struggle to provide equitable access to essential services.
This disparity is often exacerbated in low- and middle-income countries, where limited funding leads to inadequate infrastructure and workforce shortages. For instance, in many regions, out-of-pocket expenses remain a barrier, preventing individuals from seeking necessary care. Furthermore, the allocation of resources is frequently skewed, favoring urban over rural areas, further deepening health inequities.
Policies aimed at reforming healthcare financing are essential to bridging these gaps. By promoting sustainable funding models and encouraging investments in primary healthcare, countries can enhance their systems' resilience.
Ultimately, addressing these global health disparities requires a concerted effort to understand and tackle the underlying healthcare financing challenges that hinder progress.
Universal Healthcare Models
Universal healthcare models aim to provide extensive health services to all citizens, guaranteeing equitable access regardless of socioeconomic status or geographic location. These models prioritize universal access, making healthcare a right rather than a privilege. Countries like Canada and Sweden exemplify how universal healthcare can successfully reduce disparities, providing vital services without financial barriers.
To achieve healthcare sustainability, these systems rely on efficient resource allocation and preventive care measures. For instance, investing in community health initiatives not only improves population health but also reduces long-term costs associated with chronic diseases. By focusing on preventative care, countries can alleviate pressure on emergency services and hospitals, creating a more resilient health infrastructure.
Moreover, universal healthcare fosters a healthier workforce, enhancing productivity and economic growth. Evidence shows that when citizens have access to necessary medical services, overall societal health improves, leading to lower healthcare costs over time.
The challenge remains in balancing these benefits with fiscal constraints, prompting policymakers to innovate funding models that maintain sustainability while preserving quality care. Fundamentally, universal healthcare models are essential for achieving equitable health outcomes and fostering a healthier society.
Privatized Health Systems

Privatized health systems often prioritize efficiency and innovation, but they can also lead to significant disparities in access and quality of care among different population groups. When you rely on private insurance, the landscape of healthcare accessibility becomes uneven. Individuals with extensive coverage may receive timely and high-quality care, while those with minimal or no insurance face barriers that can impact their health outcomes severely.
Research indicates that privatized systems can exacerbate inequalities. In countries where private insurance predominates, lower-income individuals often struggle to afford necessary services, leading to delayed treatments and poorer health status. This disparity not only strains public health systems but also imposes additional costs on society due to the increased demand for emergency services.
To address these concerns, policymakers need to explore regulations that enhance healthcare accessibility for all citizens, regardless of their insurance status. Implementing measures like subsidies for low-income families or creating more robust public options could mitigate some of the inequities inherent in privatized systems.
Ultimately, balancing innovation with equitable access is essential for the long-term sustainability of health outcomes in privatized health systems.
Hybrid Approaches to Healthcare
Hybrid approaches to healthcare combine elements of both public and private systems, aiming to leverage the strengths of each while addressing gaps in access and quality of care. By integrating care across various settings, these systems can provide more thorough services tailored to individual needs.
You'll find that integrated care models often emphasize collaboration among healthcare providers, ensuring that patients receive coordinated treatment that enhances outcomes.
In a hybrid system, value-based healthcare plays a significant role. This approach focuses on delivering care that improves patient health at lower costs, aligning incentives for both public and private providers. For instance, when private entities are incentivized to deliver high-quality outcomes rather than simply volume, you can expect a notable shift towards efficiency and patient satisfaction.
Countries that successfully implement hybrid healthcare systems often see improved health indicators and greater patient engagement. Policies that support the integration of services can help streamline care pathways, reduce duplication of services, and enhance overall system performance.
Ultimately, hybrid approaches hold the potential to create resilient health systems capable of adapting to changing demographic and economic pressures, ensuring that everyone can access the care they need.
Key Metrics for Evaluation

Evaluating healthcare systems requires a set of key metrics that assess access, quality, efficiency, and patient outcomes to guarantee that policies are effectively meeting population health needs.
One crucial metric is health outcomes, which encompass measures like life expectancy, disease prevalence, and preventable mortality rates. These indicators help you understand how well a system is serving its population.
Another important aspect is cost efficiency. This metric evaluates how well a healthcare system utilizes its resources relative to the health outcomes achieved. By analyzing cost per capita and the cost of specific treatments, you can identify areas for improvement and ascertain that funds are allocated effectively.
Furthermore, patient satisfaction surveys provide invaluable insights into the quality of care delivered. High patient satisfaction often correlates with better health outcomes, underscoring the need for a patient-centered approach in policy formulation.
Case Studies of Select Countries
To understand the diverse approaches to healthcare, examining case studies from select countries reveals how different systems address access, efficiency, and health outcomes.
For instance, in the UK, the National Health Service (NHS) exemplifies a publicly funded model that prioritizes universal access. However, it faces country-specific challenges such as long wait times and funding constraints, necessitating ongoing reforms.
In contrast, the US operates a primarily private system, leading to significant health system comparisons. While advanced technologies and specialized care are prevalent, millions remain uninsured, highlighting disparities in access. This system struggles with high costs and administrative complexities, which could be streamlined through policy changes.
Looking at Sweden's mixed model, you'll see a robust public sector complemented by private providers, which enhances efficiency while maintaining equitable access. Yet, it grapples with balancing quality and cost amid an aging population.
These case studies illustrate that no single model is perfect; each country's health system reflects unique cultural, economic, and political contexts. Understanding these nuances helps policymakers identify best practices and tailor solutions to address specific challenges within their own healthcare landscapes.
Future Trends in Health Systems

As you explore the future of health systems, you'll notice significant opportunities in telehealth expansion and personalized medicine innovations.
These trends not only enhance access to care but also promise to tailor treatment to individual needs, improving outcomes.
Understanding the implications of these shifts will be essential for policymakers aiming to adapt health systems to evolving patient expectations and technological advancements.
Telehealth Expansion Opportunities
Telehealth is rapidly transforming healthcare delivery, offering significant opportunities to enhance access, improve patient outcomes, and reduce costs across diverse health systems globally. With the rise of remote patient monitoring, you're seeing substantial shifts in how care is provided, particularly for chronic conditions. Studies indicate that telehealth can lead to a 30% reduction in hospital admissions, driven by timely interventions through digital consultations.
Policymakers are recognizing the value of integrating telehealth into existing frameworks, as it bridges geographical gaps and addresses workforce shortages. For instance, rural populations benefit immensely from remote services, which allow them to access specialists without the burden of travel. Furthermore, insurance companies are increasingly covering telehealth services, demonstrating a commitment to innovation and accessibility.
However, challenges remain. You'll need to address regulatory barriers and guarantee that technology infrastructure is robust enough to support these services. By prioritizing investments in telehealth and fostering collaborations among stakeholders, you can create a sustainable model that not only enhances health equity but also prepares health systems for future challenges.
Embracing telehealth isn't just an option; it's a necessity for the evolving landscape of healthcare.
Personalized Medicine Innovations
Personalized medicine is revolutionizing healthcare by tailoring treatments to individual patient profiles, leveraging genetic, environmental, and lifestyle factors to enhance therapeutic efficacy and minimize adverse effects. This innovative approach relies heavily on genetic profiling, enabling healthcare providers to identify specific biomarkers that predict how a patient will respond to particular treatments.
As you explore this trend, consider how targeted therapies are reshaping treatment paradigms for conditions like cancer. These therapies focus on the unique characteristics of a patient's tumor, which can lead to improved outcomes and reduced toxicity compared to traditional, one-size-fits-all approaches.
Policymakers must prioritize investments in genomic research and data-sharing initiatives to accelerate the integration of personalized medicine into standard practice. Establishing guidelines for the ethical use of genetic information is essential to safeguard patient privacy and guarantee equitable access to advanced therapies.
To maximize the benefits of personalized medicine, healthcare systems should also facilitate multidisciplinary collaborations among geneticists, oncologists, and primary care providers. By doing so, you can help create an environment where personalized medicine thrives, ultimately leading to improved health outcomes and more efficient healthcare delivery.
Conclusion
In examining global health systems, it's clear that no single model is universally superior.
Countries with universal healthcare often achieve better health outcomes, while privatized systems can drive innovation.
However, hybrid approaches may offer a balanced solution, combining efficiency with accessibility.
As you consider future trends, focus on integrating technology and addressing social determinants of health to enhance equity.
By analyzing these diverse systems, you can better inform policies that promote effective and sustainable healthcare for all.