The World Health Organization's Health Emergencies Programme (WHE) boosts global public health readiness by emphasizing emergency preparedness and collaboration. You'll see how it effectively strengthens countries' abilities to detect and respond to health threats, as evidenced by its swift actions during the Ebola crisis and the COVID-19 pandemic. WHE also addresses health equity, ensuring vulnerable populations receive essential support during emergencies. Despite facing challenges like resource limitations and logistical hurdles, its focus remains on community engagement and sustainable solutions. If you want to explore the program's impact and future goals further, there's much more to uncover.
Overview of WHE

The World Health Organization's Health Emergencies Programme (WHE) is designed to enhance global readiness and response to public health risks, guaranteeing that we can effectively tackle outbreaks and health crises. This initiative emphasizes the importance of emergency preparedness, equipping countries with the tools and strategies necessary to respond swiftly to health threats.
By fostering collaborations among nations, WHE promotes shared knowledge and resources, creating a more resilient global health landscape.
Moreover, WHE prioritizes health equity, recognizing that vulnerable populations often bear the brunt of health emergencies. By addressing disparities in health access and outcomes, the programme aims to guarantee that all individuals receive appropriate care during crises. WHE's approach integrates data-driven assessments and evidence-based interventions, bolstering the effectiveness of emergency responses.
Incorporating community engagement is another critical aspect, as local involvement enhances preparedness and response efforts. By empowering communities, WHE helps to build trust and promotes adherence to health guidelines during emergencies.
To conclude, the WHE is an extensive framework that not only addresses immediate health threats but also lays the groundwork for sustainable, equitable health systems worldwide.
Key Objectives of the Programme
One of the primary objectives of the Health Emergencies Programme is to strengthen countries' capacities to detect, prevent, and respond to health threats effectively. By focusing on evidence-based strategies, the programme aims to enhance surveillance systems and improve early warning mechanisms. This proactive approach guarantees that countries can identify potential outbreaks before they escalate into crises.
Another key objective is fostering community engagement. Engaging local populations not only builds trust but also empowers communities to take part in their health security. By involving residents in preparedness efforts, the programme promotes a culture of resilience, guaranteeing that communities are better equipped to handle health emergencies.
Effective resource allocation is also essential. The programme emphasizes optimizing the distribution of financial, human, and technical resources to maximize impact. By strategically targeting investments, countries can strengthen their health infrastructures, guaranteeing they're prepared for future challenges.
Major Success Stories
Countries have turned around their health emergency responses remarkably, showcasing the effectiveness of the Health Emergencies Programme through various success stories.
One compelling example is the rapid containment of Ebola in West Africa. By leveraging strong community engagement, health authorities mobilized local populations to adhere to preventive measures, greatly reducing transmission rates. Success metrics, such as decreased infection and mortality rates, underscore this achievement.
Another success story is the swift response to the COVID-19 pandemic in several nations. Countries that implemented the Health Emergencies Programme effectively established transparent communication channels, allowing them to disseminate accurate information quickly. This transparency fostered trust, leading to high vaccination rates and compliance with health guidelines.
Moreover, in regions facing natural disasters, the programme's emphasis on preemptive planning and community involvement has proven essential. Communities participated in risk assessments and resource allocation, enhancing resilience.
These examples highlight how the Health Emergencies Programme not only improves immediate responses but also builds long-term capacity through community engagement. By focusing on success metrics, we can see the tangible impact of these initiatives in saving lives and strengthening health systems globally.
Challenges in Implementation
Implementing the Health Emergencies Programme faces significant challenges that can hinder its effectiveness, including insufficient resources, varying political commitment, and disparities in healthcare infrastructure.
Funding limitations severely restrict the ability to mobilize fundamental resources, leaving gaps in preparedness and response capacities. Without adequate financial support, health systems struggle to maintain operational efficiency during emergencies.
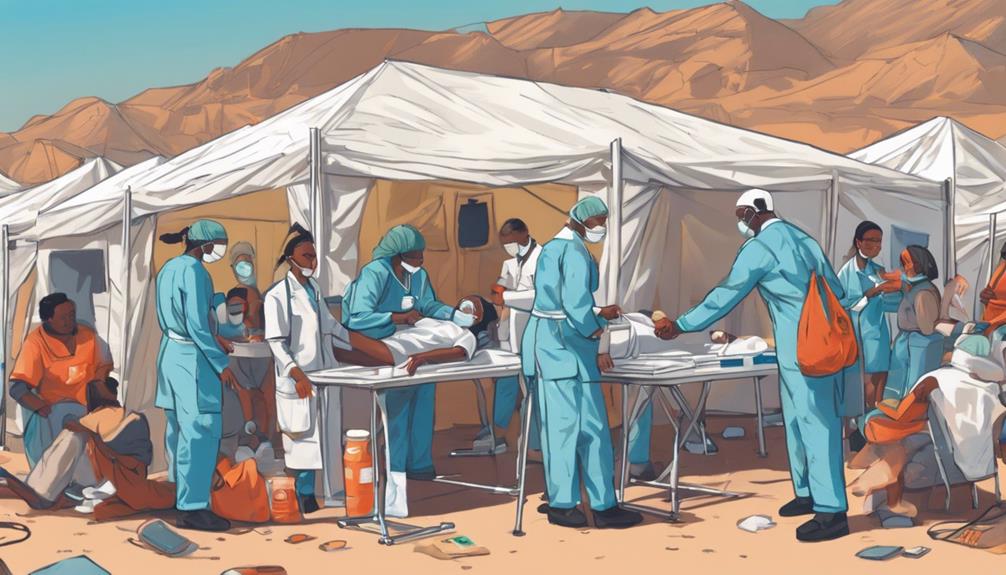
Logistical hurdles further complicate implementation. Difficulties in coordinating supply chains are essential for delivering medical supplies and personnel to affected areas. These challenges can delay response times, exacerbating health crises.
Moreover, stakeholder engagement is critical yet often inconsistent. Engaging local communities, governmental bodies, and international partners requires careful navigation of different interests and agendas. If stakeholders aren't aligned, efforts can fragment, undermining the program's objectives.
Lastly, policy alignment across various levels of government is necessary for cohesive action. Disparate policies can lead to miscommunication and ineffective strategies, ultimately impacting the program's success.
Addressing these challenges is vital for enhancing the Health Emergencies Programme's impact and ensuring a robust response to future health crises.
Global Collaboration Efforts

Global collaboration is essential for enhancing the effectiveness of the Health Emergencies Programme, as it facilitates resource sharing, knowledge exchange, and coordinated responses during health crises.
By fostering cross-border partnerships, countries can tackle health challenges more efficiently. Consider how nations have teamed up to combat outbreaks like Ebola and COVID-19. These collaborations allow for pooling resources, such as medical supplies and personnel, which can prove crucial during emergencies.
When you engage in cross-border partnerships, you're not just sharing resources; you're also exchanging best practices and information. This exchange is critical for understanding disease transmission dynamics and developing effective intervention strategies. For instance, countries can share real-time data on infection rates, allowing for timely responses that can save lives.
Furthermore, coordinated responses reduce duplication of efforts, ensuring that resources are allocated where they're needed most. The effectiveness of the Health Emergencies Programme hinges on these collaborative efforts, as they create a more resilient global health system.
In a world where health threats easily cross borders, your commitment to international cooperation is paramount to safeguarding public health.
Impact on Vulnerable Populations
Vulnerable populations often bear the brunt of health emergencies, facing heightened risks due to limited access to healthcare, socioeconomic disparities, and pre-existing health conditions. These health disparities become more pronounced during crises, as emergency preparedness plans frequently overlook the unique needs of marginalized groups. Social determinants like income, education, and housing quality create significant access barriers that impede effective healthcare delivery.
The impact of health emergencies on these populations extends beyond physical health; mental health suffers too. Increased stress, anxiety, and depression can arise from inadequate resources and support systems during crises. To enhance community resilience, targeted resource allocation is essential, ensuring vulnerable groups receive appropriate care and resources during emergencies.
Moreover, the policy implications of addressing these issues are profound. Policymakers must prioritize inclusive strategies that consider the needs of all communities in emergency planning. By fostering equitable access to healthcare and addressing the underlying social determinants of health, we can mitigate the adverse effects of health emergencies on vulnerable populations.
Ultimately, a focused approach not only protects these communities but strengthens the overall health system, making it more resilient for future challenges.
Future Directions and Goals

As health emergencies evolve, it's essential to establish clear goals that prioritize equitable access to care and address the unique challenges faced by marginalized communities.
Achieving health equity means recognizing the disparities in health outcomes and actively working to reduce them. This requires implementing targeted interventions that focus on the most vulnerable populations, ensuring that everyone has the resources they need during crises.
To reach these objectives, sustainable funding is imperative. Without stable financial support, programs designed to enhance health equity will struggle to maintain their effectiveness. By advocating for long-term investments, you can help secure the necessary resources to support initiatives that provide immediate relief and build resilience in communities.
Moreover, collaboration with local organizations can amplify the impact of these efforts. Engaging stakeholders who understand the specific needs of their communities is essential for developing tailored solutions.
As you push for future directions in health emergencies, remember that integrating equity into every aspect of planning and response is key to fostering a fairer healthcare landscape. By focusing on health equity and securing sustainable funding, you're contributing to a healthier, more equitable world for everyone.
Conclusion
In conclusion, the WHO's Health Emergencies Programme plays an essential role in enhancing global health security.
Its key objectives, demonstrated successes, and collaborative efforts showcase its effectiveness in addressing health crises, particularly for vulnerable populations.
However, challenges persist, requiring ongoing adaptation and innovation.
As you consider the future directions of this program, it's clear that sustained commitment and global cooperation will be essential in mitigating health emergencies and improving resilience worldwide.